What is Breast Cancer?
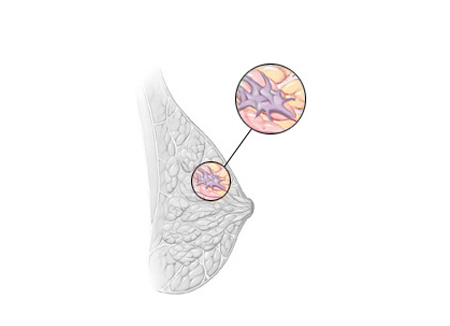
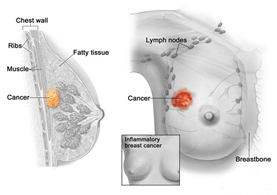
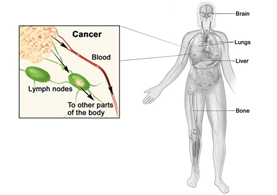
Breast cancer is a malignant (cancer) tumor that starts in the cells of the breast, can invade surrounding tissues or metastasize to distant areas of the body.1
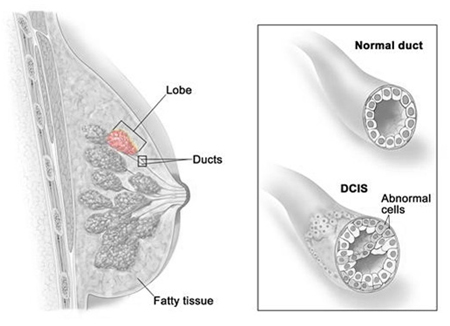
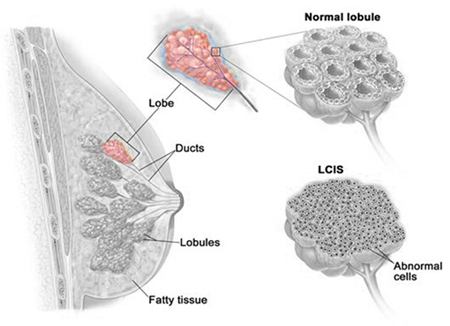
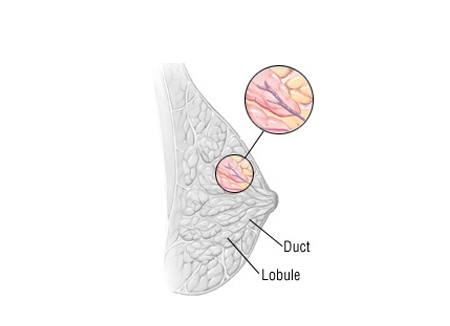
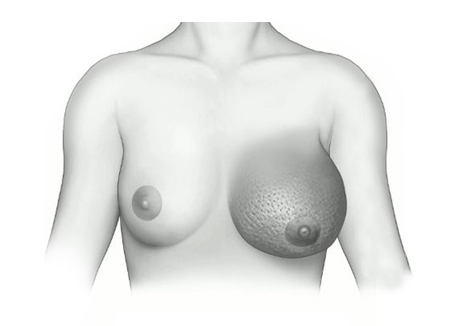
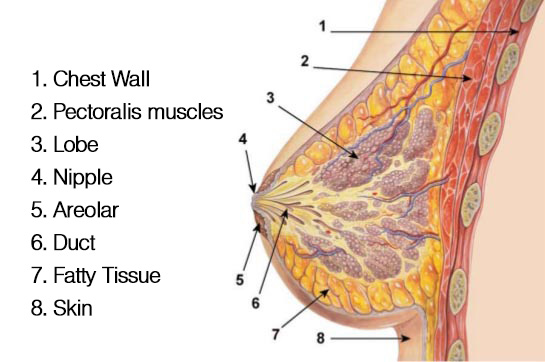
Breast Anatomy
How common is it in India?
Breast cancer is the most common cancer among women in India and worldwide Over 1,00,000 new breast cancer cases are estimated to occur every year and over 50,000 women are estimated to die of it annually in India.2,3
Which are the types of Breast Cancer?
Breast tumors can be benign or malignant. Benign breast lumps are cysts, fibroadenomas and intraductal papillomas.1
Types of breast cancer:1
Risk factors involved in Breast Cancer1
- Gender: Breast cancer is much more common in women than in men.
- Age: Risk goes up with age.
- Genetic risk factors: Inherited changes (mutations) in certain genes like BRCA1 and BRCA2 can increase the risk.
- Family history: Breast cancer risk is higher among women whose close blood relatives have this disease.
- Personal history of breast cancer: A woman with cancer in one breast has a greater chance of getting another breast cancer.
- Race: Overall, white women are slightly more likely to get breast cancer than African-American women. African-American women, though, are more likely to die of breast cancer.
- Dense breast tissue: Dense breast tissue means there is more gland tissue and less fatty tissue. Women with denser breast tissue have a higher risk of breast cancer.
- Certain benign (not cancer) breast problems: Women who have certain benign breast changes may have an increased risk of breast cancer.
- Menstrual periods: Women who began having periods early (before age 12) or who went through menopause (stopped having periods) after the age of 55 have a slightly increased risk of breast cancer.
- Breast radiation early in life: Women who have had radiation treatment to the chest area (as treatment for another cancer) as a child or young adult have a greatly increased risk of breast cancer.
- Treatment with DES: Women who were given the drug DES (diethylstilbestrol) during pregnancy have a slightly increased risk of getting breast cancer.
- Not having children or having them later in life: Women who have not had children, or who had their first child after age 30, have a slightly higher risk of breast cancer. Being pregnant many times or pregnant when younger reduces breast cancer risk.
- Certain kinds of birth control: Studies have found that women who are using birth control pills or an injectable form of birth control called depot-medroxyprogesterone acetate (DMPA) have a slightly greater risk of breast cancer than women who have never used them.
- Using hormone therapy after menopause: Taking estrogen and progesterone after menopause (sometimes called combined hormone therapy) increases the risk of getting breast cancer.
- Not breastfeeding: Some studies have shown that breastfeeding slightly lowers breast cancer risk, especially if breastfeeding lasts 1½ to 2 years.
- Alcohol: The use of alcohol is clearly linked to an increased risk of getting breast cancer. Even as little as one drink a day can increase risk.
- Being overweight or obese: Being overweight or obese after menopause (or because of weight gain that took place as an adult) is linked to a higher risk of breast cancer.
Stages of Breast Cancer4
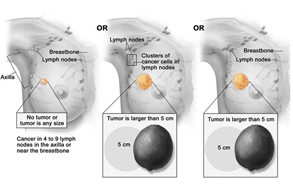
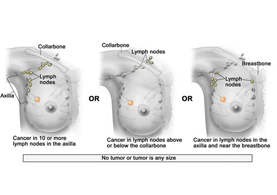
TNM (T- Tumor size, N- Lymph node invasion, M- Metastasis) Classification of Breast Cancer
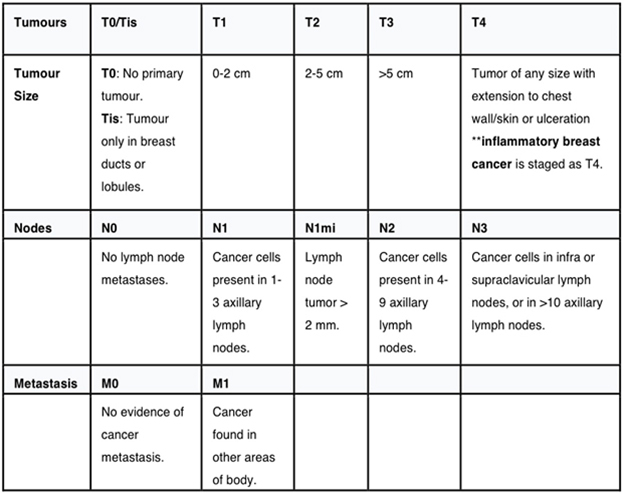
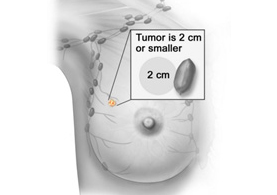
Stage I breast cancer. T1,N0,M0
Tumor is less than 2 cm with or without micrometastases in lymph node
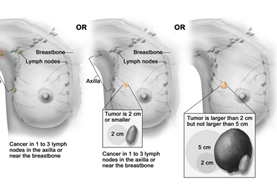
Stage IIA - T0, N1,M0 OR T1,N1,M0 OR T2,N0,M0
Tumor is less than 2 cm in size with 3 axillary lymph node involvement or tumor is of 5 cm in size
Stage IIB – T2,N1,M0 OR T3,N0,M0
Tumor is larger than 2cm but not more than 5cm in size and involve 1-3 axillary lymphnodes
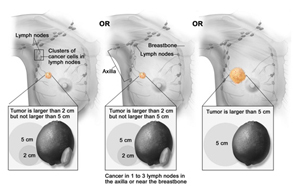
Stage III A - T0,N2,M0 OR T3,N1,M0 OR T3,N2,M0
Tumor that involves either 4-9 axillary lymph nodes or > 5 cm in size and involves up to 9 axillary lymph nodes
How one can find Breast Cancer in early disease?
Screening Methods for Breast Cancer1
Clinical Breast Exam (CBE) and Breast Self Exam (BSE)
- Monthly BSE for all women aged 20 years.
- CBE every 3 year for 20-39 year age, every year for 40 year age and above.
Mammography1
- Women ages 40 to 44 should have the choice to start annual breast cancer screening with mammograms if they wish to do so.
- Women age 45 to 54 should get mammograms every year.
- Women age 55 and older should switch to mammograms every 2 years, or have the choice to continue yearly screening.
MRI5
Women who are at high risk for breast cancer based on certain factors should get an MRI and a mammogram every year. This includes women who:
- Have a lifetime risk of breast cancer of about 20% to 25% or greater, according to risk assessment tools that are based mainly on family history.
- Have a known BRCA1 or BRCA2 gene mutation.
- Have a first-degree relative (parent, brother, sister, or child) with a BRCA1 or BRCA2 gene mutation, and have not had genetic testing themselves.
- Had radiation therapy to the chest when they were between the ages of 10 and 30 years.
Signs and Symptoms of Breast Cancer1
- Swelling of all or part of the breast.
- Skin irritation or dimpling.
- Breast pain.
- Nipple pain or the nipple turning inward.
- Redness, scaliness, or thickening of the nipple or breast skin.
- A nipple discharge other than breast milk.
Which are the treatment options for Breast Cancer?
Treatment of Breast Cancer5
 Surgery
Surgery
 Radiation therapy
Radiation therapy
 Chemotherapy
Chemotherapy
 Hormone therapy
Hormone therapy
 Targeted therapy
Targeted therapy
 Surgery:
Surgery:
- BCS (Breast Conservative Surgery): Partial mastectomy, Lumpectomy- removes only a part of the breast.
- Mastectomy: If just the breast is removed (and not lymph nodes under the arm) it is called a simple (or total) mastectomy. A simple mastectomy combined with an axillary lymph node dissection (discussed below) is called a modified radical mastectomy.
- Skin-sparing mastectomy: For some women considering immediate reconstruction, skin-sparing mastectomy can be done. In this procedure, most of the skin over the breast (other than the nipple and areola) is left intact.
- Radical mastectomy: In this operation, the surgeon takes a modified radical mastectomy one step further by also removing the muscles of the chest wall under the breast. This is only needed if the cancer is growing into the muscles under the breast.
- Axillary lymph node dissection: In this operation, about 10 to 40 (though in most cases less than 20) lymph nodes are removed. Axillary lymph node dissection is usually done at the same time as the mastectomy or breast-conserving surgery.
- Sentinel lymph node biopsy: A sentinel lymph node biopsy is a way to learn if cancer has spread to the lymph nodes under the arm without removing so many of them. For this test, a radioactive substance and/or a blue dye are injected into the breast. This is carried by the lymph system to the nodes that first get lymph from the tumor. These lymph nodes (called the sentinel lymph nodes) are also the one most likely to contain cancer cells if the cancer has spread. The surgeon then removed the nodes containing the blue dye or radiation.
 Radiation therapy for breast cancer55
Radiation therapy for breast cancer55
Radiation therapy is treatment with high-energy rays (such as x-rays) or particles to kill cancer cells. Radiation therapy may be used to kill cancer cells remaining in the breast, chest wall, or underarm area after surgery or, less often, to shrink a tumor before surgery. Radiation to the breast is often needed after breast-conserving surgery. Radiation may also be recommended after mastectomy in patients either with a cancer larger than 5 cm, or when cancer is found in the lymph nodes.It is usually given after any chemotherapy. Radiation is also used to treat cancer that has spread to other areas, for example to the bones or brain.
 Chemotherapy5
Chemotherapy5
Chemotherapy (chemo) is the use of cancer-killing drugs. These drugs can be put into a vein, given as a shot, or taken as a pill or liquid. They enter the bloodstream and reach most parts of the body, making this treatment useful for cancers that have spread to distant organs. While these drugs kill cancer cells, they also damage some normal cells, which can lead to side effects.
Chemo can be used either before or after surgery for early-stage breast cancer. This is to kill any cancer cells that may have spread but are too small to be seen by exam or tests.
- When chemo is given after surgery to patients who have no signs of cancer spread it is called adjuvant chemo. This lowers the chance of the cancer coming back later.
- When chemo is given before surgery to cure the cancer it is called neoadjuvant chemo. This can shrink large cancers so that they are small enough to be removed with breast-conserving surgery instead of mastectomy. It also works as well as adjuvant chemo in lowering the chance that the cancer will come back later.
Chemo can also be used as the main treatment for women with cancer that has spread to distant sites (outside the breast and the nearby lymph nodes).
 Hormone therapy : (ESMO guidelines)5,6
Hormone therapy : (ESMO guidelines)5,6
- Premenopausal patients: Tamoxifen 20 mg/day for 5–10 years.
- In patients becoming postmenopausal during the first 5 years of tamoxifen, a switch to letrozole, an aromatase inhibitor (AI), seems to be particularly beneficial.
- Postmenopausal patients: Aromatase inhibitors.
 Targeted therapy
Targeted therapy
Most of the targeted drugs used to treat breast cancer target HER2/neu. In some patients, their breast cancer cells have too much of this protein. Certain drugs target this protein, stopping it from causing breast cancer cell growth. These are trastuzumab, pertuzumab, ado Trastuzumab emtansine and lapatinib.
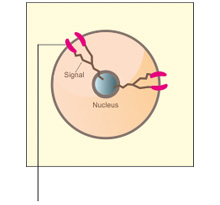
What is HER2 positive breast cancer?
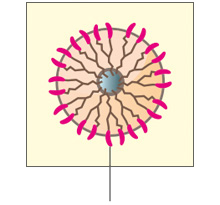
- The HER2 (human epidermal growth factor receptor 2) gene encodes the receptor tyrosine kinase HER2 and is often over-expressed in breast cancer. Increased number of HER2 contributes to tumor progression.7
- Breast cancers can have up to 25–50 copies of the HER2 gene, and up to 40–100 fold increase in HER2 protein resulting in 2 million receptors expressed at the tumor cell surface.8
- Increased HER2 signaling plays a role in increasing proliferation and survival of the primary tumor and distant lesions which upon completion of full transformation cause metastases.8
- HER2-positive breast cancer is considered aggressive because it grows and spreads quickly.9
- Approximately 1 in 5 patients with breast cancer has HER2-positive breast cancer.9,10
Accurate HER2 testing is extremely important. HER2 testing is done by immunohistochemistry (IHC) assay and by in situ hybridization (ISH) assay on a breast cancer specimen.11
If you are HER2-positive, you can potentially benefit from a therapy that targets HER2.
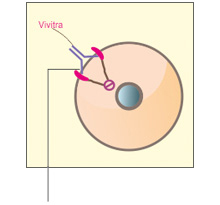
What is VivitraTM (Trastuzumab)?
VivitraTM (Trastuzumab) is a highly biosimilar medicinal product of reference biologic. It is a humanized monoclonal anti-HER2 (Human epidermal growth factor receptor 2) antibody.12
Metastatic Breast Cancer (MBC): VivitraTM (Trastuzumab) is indicated for the treatment of patients with HER2 overexpressing metastatic breast cancer. VivitraTM (Trastuzumab) is also indicated in combination with aromatase inhibitor for the treatment of patients with HER2 overexpressing and hormone receptor-positive metastatic breast cancer.12
Early Breast Cancer (EBC): VivitraTM (Trastuzumab) is indicated for the treatment of patients with HER2 overexpressing early breast cancer following surgery, chemotherapy (neo adjuvant or adjuvant) and radiotherapy (if applicable). VivitraTM (Trastuzumab) is also indicated for adjuvant treatment of patients with HER2 overexpressing node positive or node negative breast cancer i) as part of treatment regimen comprising doxorubicin, cyclophosphamide, and either paclitaxel or docetaxel ii) with docetaxel and carboplatin.12
References
- Breast cancer overview, American cancer society. Available on www.cancer.org/breast-cancer-overview-pdf last accessed on november 2015.
- Globocan 2012 available on http://globocan.iarc.fr/Pages/fact_sheets_population.aspx last accessed on november 2015.
- Parveen Kumar, Nityanand B. Bolshette et al .Breast cancer status in India:Overview Biomedicine & Preventive Nutrition 3 (2013) 177–183.
- AJCC TNM classification Cancer Staging manual , edition 7th.
- Breast cancer- American cancer society available at www.cancer.org/acs/groups/cid/documents/webcontent/003090-pdf.pdf accessed on november 2015.
- Senkus E, Kyriakides S, Ohno S, Penault-Llorca F, Poortmans P, Rutgers E,Zackrisson S, Cardoso F; ESMO Guidelines Committee. Primary breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015 Sep;26 Suppl 5:v8-30.
- Freudenberg JA, Wang Q, Katsumata M, Drebin J, Nagatomo I, Greene MI. The role of HER2 in early breast cancer metastasis and the origins of resistance to HER2-targeted therapies. Exp Mol Pathol. 2009 Aug;87(1):1-11.
- Gutierrez C, Schiff R. HER2: biology, detection, and clinical implications. Arch Pathol Lab Med. 2011 Jan;135(1):55-62.
- Pegram M, Slamon D. Biological rationale for HER2/ neu (c-erbB2) as a target for monoclonal antibody therapy. Semin Oncol. 2000;27(suppl 9):13-19.
- HER2 status. Breastcancer.org. http://www.breastcancer.org/symptoms/diagnosis/her2. Updated March 10, 2015. Accessed on november 2015
- ASCO 2013 Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, Allred DC, Bartlett JM, Bilous M, Fitzgibbons P, Hanna W, Jenkins RB, Mangu PB, Paik S, Perez EA, Press MF, Spears PA, Vance GH, Viale G, Hayes DF; American Society of Clinical Oncology; College of American Pathologists. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013 Nov 1;31(31):3997-4013
- VivitraTM (Trastuzumab) Prescribing Information.